Pleural Effusions: Transudate vs. Exudate
Classifying Pleural Effusions
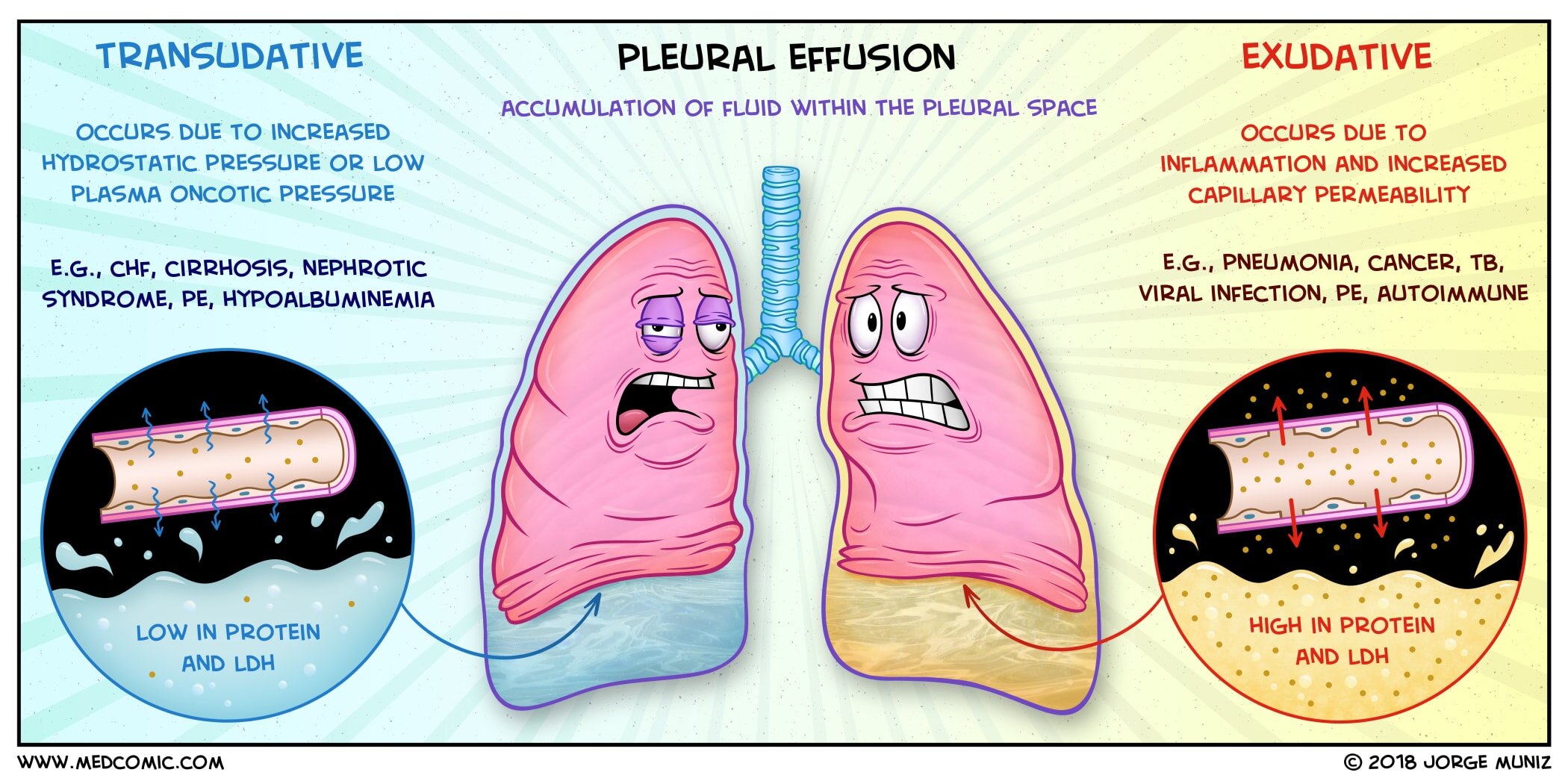
A pleural effusion is an accumulation of fluid within the pleural space
Determining the underlying cause is facilitated by thoracentesis and pleural fluid analysis
The pleural fluid may be classified as a transudate or an exudate, depending on the etiology
Transudates occur secondary to conditions which cause an increase in the pulmonary capillary hydrostatic pressure or a decrease in the capillary oncotic pressure
Leads to accumulation of protein poor pleural fluid
Common causes include: CHF, nephrotic syndrome, cirrhosis, hypoalbuminemia, pulmonary embolism
Exudates occur secondary to conditions which cause inflammation or increased pleural vascular permeability
Leads to accumulation of protein rich pleural fluid and cells
Common causes include: pneumonia, cancer, tuberculosis, pulmonary embolism
According to Light’s criteria, if at least one of the following criteria is present, then the fluid is determined to be an exudate:
Pleural fluid protein to serum protein ratio greater than 0.5
Pleural fluid LDH to serum LDH ratio greater than 0.6
Pleural fluid LDH greater than two-thirds the upper limit for normal serum LDH
Presentation
Often asymptomatic, but can present with dyspnea, pleuritic chest pain, and cough
Physical examination may demonstrate decreased breath sounds on the side of the effusion, dullness to percussion, and decreased tactile fremitus
Imaging
Chest x-ray: blunting of costophrenic angles; free-flowing effusions will result in layering of fluid on the decubitus view
Chest CT sometimes used for further evaluation
Treatment
Treat underlying cause
Thoracentesis is diagnostic and therapeutic
Pleurodesis or indwelling catheter for recurrent/malignant effusions