Clostridium difficile Infection
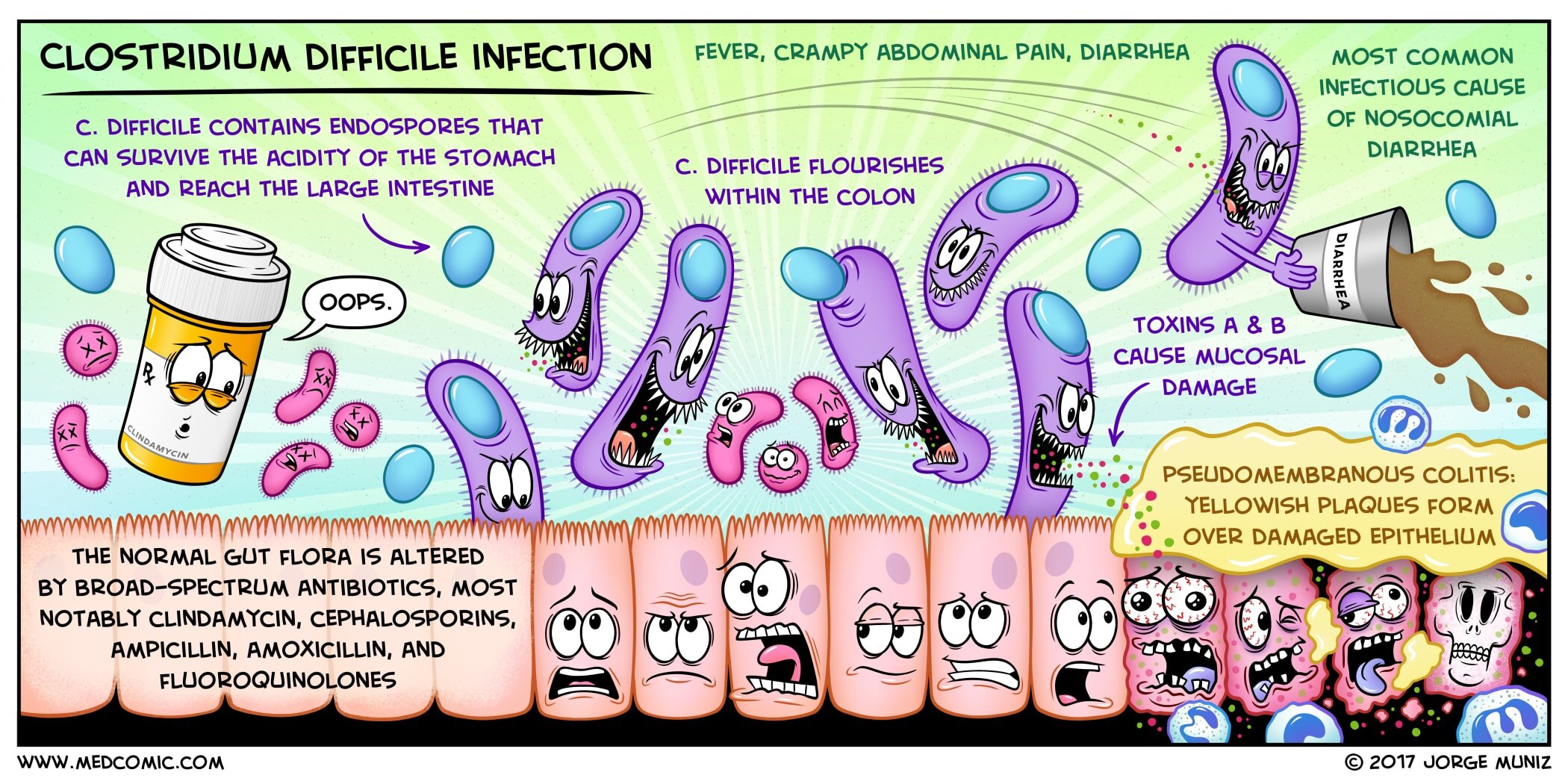
Clostridium difficile is a gram-positive anaerobic bacillus which secretes toxins (A and B) that cause diarrhea and pseudomembranous colitis. C. difficile is the most common infectious cause of nosocomial diarrhea. Transmission of C. difficile can occur from contact with contaminated humans and fomites. The organism contains endospores that can survive the acidity of the stomach and reach the large intestine.
C. difficile colonizes the intestinal tract after the normal gut flora has been altered by antibiotic therapy. It can flourish after any antibiotic therapy, but most notably occurs with broad-spectrum antibiotics such as clindamycin, cephalosporins, ampicillin, amoxicillin, and fluoroquinolones. Pseudomembranous colitis is an inflammatory bowel disorder in which yellowish plaques form over the damaged intestinal mucosa. The plaque is an exudate that resembles a membrane, hence the term “pseudomembranous.”
The signs and symptoms include fever, crampy abdominal pain, and diarrhea. Progression of the condition can lead to leukocytosis, dehydration, and toxic megacolon. The diagnosis is confirmed with a stool assay for C. difficile toxin. Pseudomembranes can be seen on sigmoidoscopy.
Treatment includes discontinuing the causative agent. Oral metronidazole is the treatment of choice in patients that do not respond to conservative measures. Alternatively, very severe cases may require oral vancomycin. Rarely, cases complicated by toxic megacolon or perforation may require total colectomy.