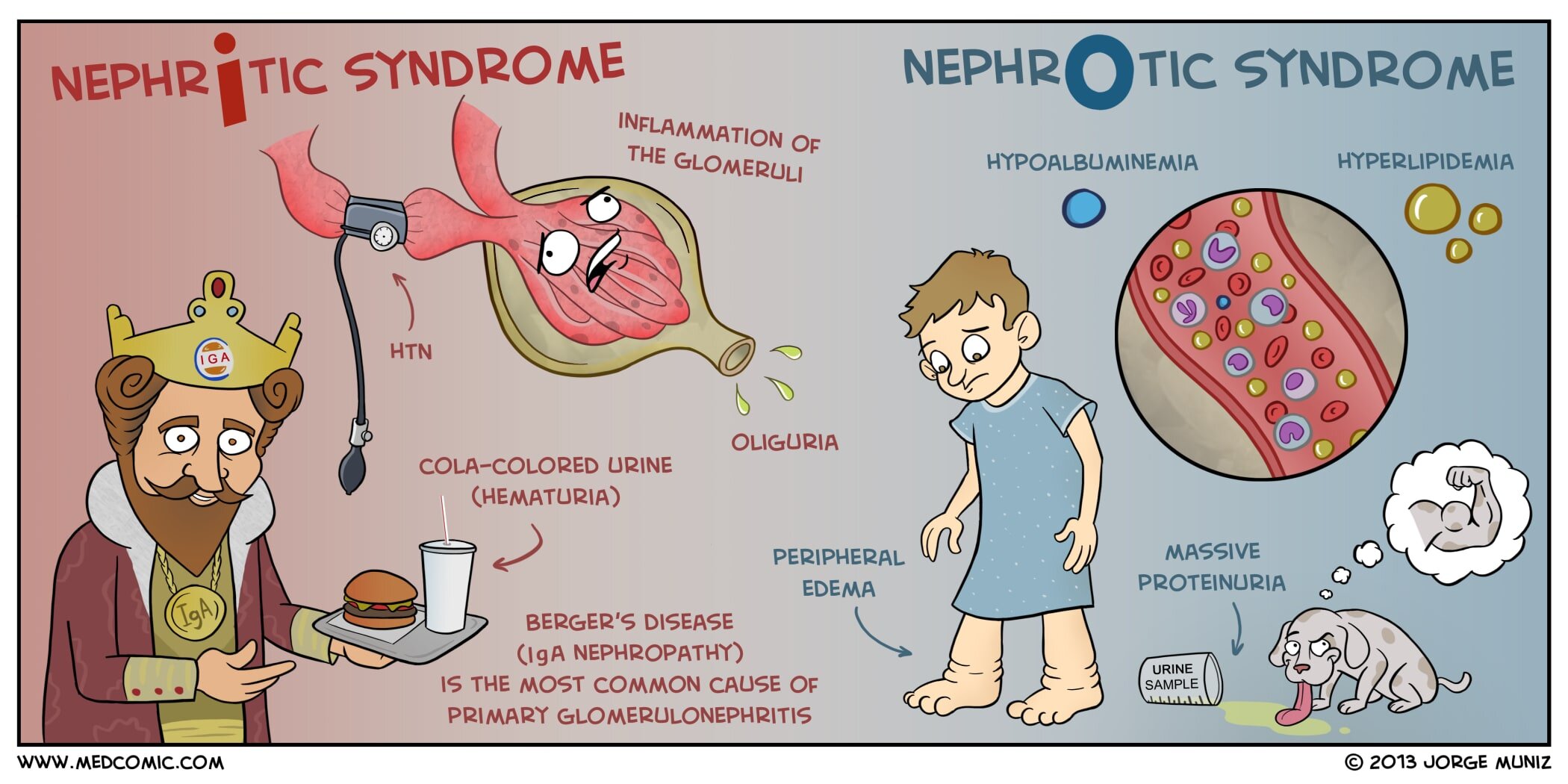
Nephritic vs. Nephrotic Syndrome
Nephritic syndrome is characterized by inflammation of the glomeruli (glomerulonephritis) and renal dysfunction. The most common cause is immunoglobulin A (IgA) nephropathy, also known as Berger’s disease, but other causes include postinfectious glomerulonephritis and lupus nephritis. Nephritic syndrome can present with oliguria, hypertension, and hematuria (cola-colored urine). Edema may also be present, although it is not nearly as severe as in nephrotic syndrome. Laboratory findings include hematuria, proteinuria (< 3.0 g/day), elevated BUN and creatinine, and red cell casts in urine.
Nephrotic syndrome develops as damage to glomeruli results in massive proteinuria and generalized edema (anasarca). It can be caused by a variety of disorders in adults (e.g., diabetes mellitus, amyloidosis, systemic lupus erythematosus (SLE), and focal segmental glomerulosclerosis). The most common cause in children is minimal change disease. The edema of nephrotic syndrome decreases the amount of intravascular fluid and decreases blood pressure, stimulating the kidneys to release renin. Ultimately, the adrenal glands respond by releasing aldosterone to retain sodium and water, which provides more fluid to contribute to the further development of edema. Laboratory findings include hypoalbuminemia, massive proteinuria (> 3.5 g/day), hyperlipidemia, and waxy casts and oval fat bodies in urine.